The power of data and integration in health, care and public services
Data and collaboration in early 2020

I still get the shivers thinking back to it now. It’s early March 2020, I’m in the unfortunate position as a doctor training in public health in Welsh Government, and am wracking my brains trying to work between government, our Welsh public health and digital health agencies and the professions as we try to accelerate access to data on people infected with COVID-19 and how the pandemic is affecting the health system.
We all know health planning and data is too hospital-focussed, for reasons that are many: institutional biases towards secondary care, funding, ease of access to such data and like others. But that excuses in no way the derisory skew in the modelling done from January and February 2020 that omitted how communities and community services themselves would be affected. We were determined to address that; I don’t think though we got close to meeting half of our aspirations.
A bit about me
Let me go back a few steps. I’ve been working as a doctor between primary care and public health since 2015. Training across both roles was I’m told illegal (still waiting for the charges..) and against the Medical Act of 1983, until independence from the EU apparently allowed us to forge our own way in postgraduate health training, making the approved dual general practice/public health training pathway possibly the single, only positive dividend of Brexit and divergence from the EU. Anyway.
Soon into public health training it became apparent few advanced methods in data science or new digital technologies were part of our training. We regard ourselves as fairly rigorous people when it comes to evidence-based practice and health statistics – possibly even so far as the evidence-based health police, passively remarking on the lack of strong research evidence for what are probably most health interventions unless you’re referring to single-disease drug treatments. Which isn’t entirely helpful if nobody is investing in the evidence-base for public health interventions, which thankfully people are, but they’ll never meet the investment of drug and technology corporations. Enter data.
Data science in public health training
My first foray into data science was pretty accidental. An academic lecturer nudged me away from my initial dissertation topic, steering me to a re-analysis of a previous piece of work, only for him to walk off and declare though, after I had opted to pursue the idea, that he wouldn’t be supervising me as he already had a Masters student. (The fact I’m writing this blog probably suggests I should let go of any bemusement then experienced). The data we were working with was large datasets in mortality, merging funding data across England from multiple sources, to explore whether changes in funding in local areas were linked with inequalities in rates of people dying from conditions the healthcare system can usually treat. This analysis showed us NHS funding can help narrow inequalities, but that changes in funding policy had limited previous, better efforts.
After learning some basic R coding language, my interest rose, leading me to work on a number of projects: understanding demand on acute medical services in secondary care, decomposing inequalities in life expectancy at birth in Wales by condition and age-group, exploring what proportion of inequalities in life expectancy are avoidable in Wales by good public health policy and quality healthcare, and more recently understanding the relationship between GP practice funding and deprivation in Wales. What’s been clear is that in public health we’re only skimming the surface of what’s possible in data science and engineering, and are probably neither attracting industry talent to achieve more of what’s possible, nor engaging enough in such fields to learn and share expertise.
Learning from the COVID-19 pandemic
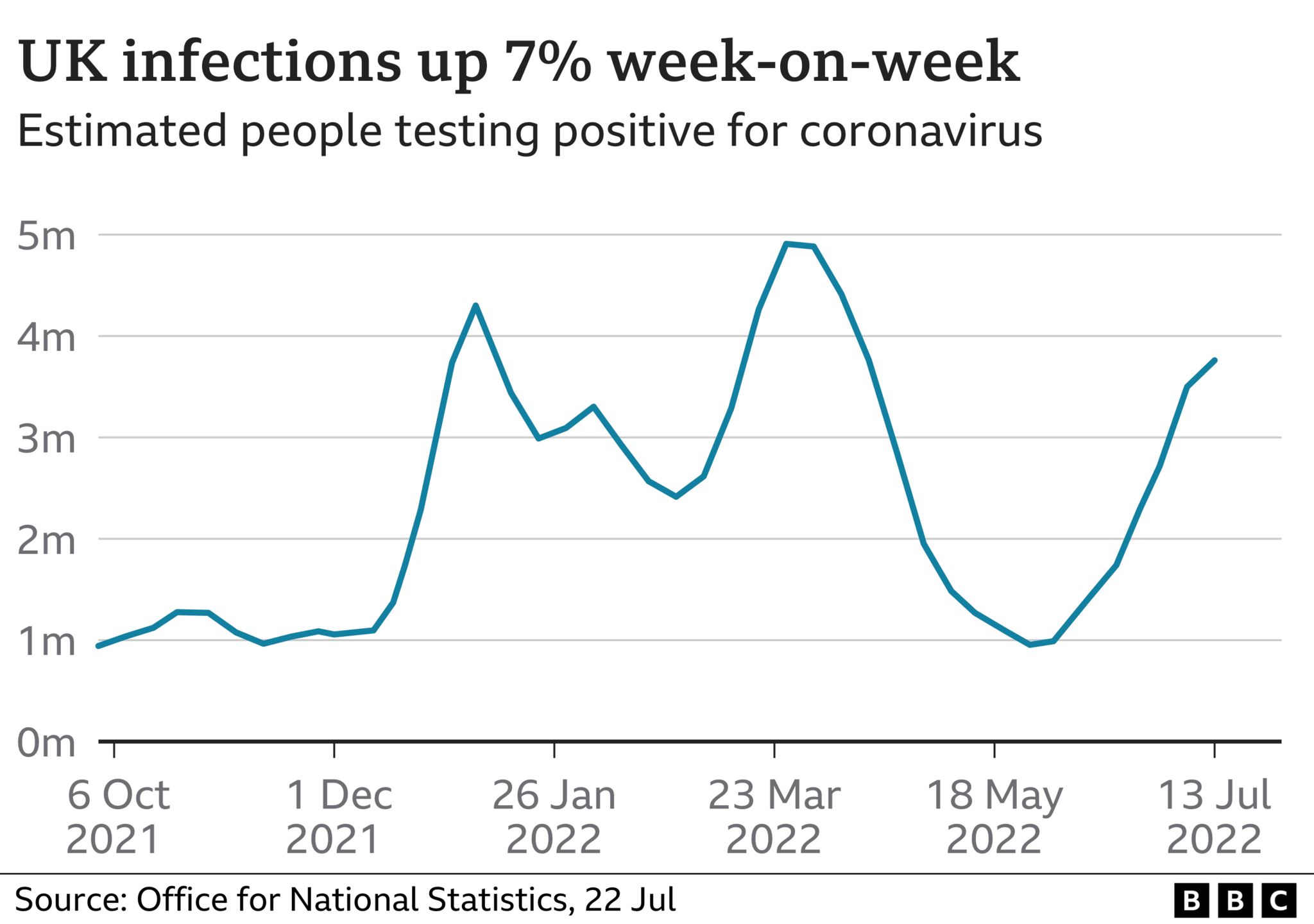
Back to March 2020. While it’s viscerally painful for many of us to remember, I hoped we’d learned some things from the pandemic. Data was key in the first wave of understanding the scale of the problem, forecasting (where possible) what demand services could expect, feeding back in real-time what was happening, and sharing this data widely across services to feed into emergency planning. As time went on, I think we saw increased public engagement in data, with open dashboards with data available to anyone with a laptop and time (there were many of those, with the economy shut) able to lend scrutiny. It’s possible some public health actions were reinforced in social distancing as the public saw what rates in their areas were doing – hammering home the point that to inform action, data needs to be clear to understand, in real-time, detailed or granular enough that people can see why it is relevant to them, and be linked to a clear action that is either encouraged, expected or enforced. Is that the kind of data we present to the public in peacetime? I’m not so sure.
The COVID inquiry is going on without much in the way of attention right now. Have we learned enough for the next time? I’d love to see a data preparedness plan, of how agencies share data in a pandemic or emergency, what structures are needed to evaluate that data, what population wellbeing measures do we need to focus on (it might be child safeguarding, educational engagement or people’s resilience are more important in an emergency than hospital occupancy rates), and how we could truly involve the public at a local level alongside statutory services.
HCB Associates Ltd – a public health and healthcare consultancy focussed on data, evidence and collaboration

I’m a GP now in the eastern outskirts of Newport. We’re building a wellbeing centre between the NHS and council aiming to deliver integrated, preventative services to a population of around 20,000. Data is key to what we do, and I think we’ve a lot to share around how citizen engagement, partnerships not only with the public sector but with business, charities and community groups and sound systems for data and innovation are key.
To support this work myself and some colleagues have set up HCB Associates, a consultancy looking to provide digital health intelligence and strategy development support to NHS, public sector and private organisations. With the rapid rise in health tech and AI, I’m keen we apply some public health principles to the field, remember who ought to benefit most from innovation, and not forget data is only as powerful as who it is collected on, recognising service data is innately biased by variation in utilisation between social groups. Finally, if we are going to use health and care data to tackle inequalities, we need to do so much more in collaboration with communities, and should work far harder to widen access to work in the industry for those in backgrounds who may tend not to benefit.
If anyone would like to work with us or has a project you’d like public health and clinical experience on, get in touch. Maybe if we collaborate more, the next time another March 2020 comes around, we’ll have a plan that gets us through the initial mess again.
Jonny, Co-Director HCB Associates