Public health in the Americas
The People’s Health Assembly 5, Mar Del Plata
Writing this from a coffee shop in Buenos Aires. It’s a rainstorm outside; I and many others are hiding from the elements, me personally given my lack of an umbrella, my sightseeing plans literally rained on by the weather.
Enough of my climate woes. I’m in Argentina to attend the 5th People’s Health Assembly , an event organised every 5 years by activists in the People’s Health Movement , a global network of grassroots health organisations from countries across the global South and North. The assembly is next week, giving me a bit of time to see some of the rest of the country (vanishingly little unfortunately, given the geography of Argentina), and learn a little about the history, politics and contexts that have shaped public health and healthcare in the Americas.

Politics and public health
Ever since I first got involved in global and public health in university, I’ve been intrigued by some of the continent’s approaches. Yes, there’s a fair amount of romanticised idealism for the continent’s politics, exemplified probably by what was once some ubiquitous imagery of a certain Argentinian doctor and military leader who played a pivotal role in the Cuban revolution.
Still, countries of the Latin American continent have demonstrated some genuinely effective policies and innovations when it comes to public health. Could that be due to their relative independence liberation from its colonial rulers in the 19th century, the freedom borne out of autonomy from the US and post-war global economic and development institutions? Or perhaps it’s been in some cases a genuine commitment to social goals, or even (lacking resources for expensive services) necessity.
Anyway, as we’ll see in the next few blogs, there is much we can learn when it comes to public health and healthcare from Latin America, particularly for those interested in the delivery of preventative, community-orientated and integrated services. Let’s start though with some data to help us understand which countries to focus on.
Life expectancy in the Americas
To understand the state of public health in the Americas, how it’s changed over the years, and how it fares compared with other regions around the world, we’re going to draw on data from the World Bank’s Open Data platform .
The chart below shows the trend in life expectancy at birth for Latin American countries, compared with the regional average in Europe/Central Asia and North America, for data available between 1960-2021. Several of the countries have seen some impressive rises during the period, likely as a result both of changes in people’s diet, income, education, and a whole lot more, as well as the healthcare services in each country.
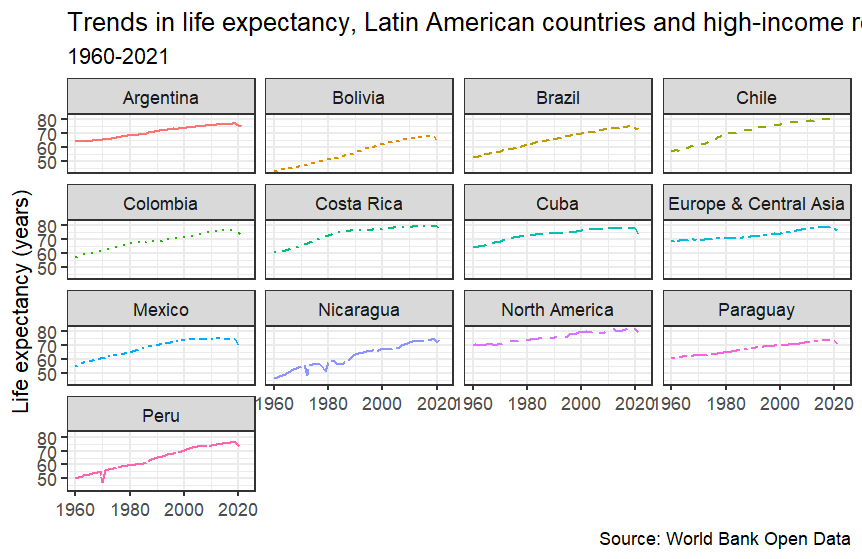
When we factor in though the wealth differences between the country’s - Nicaragua for instance only generated $2255 per person in 2022, Peru $7125 per person and Brazil $8917 per person, compared with the $27536 per person generated on average in 2022 by countries in Europe and Central Asia, or even the staggering $74161 in countries in North America, there’s clearly something impressive going on here. What are some of these countries doing that, without anywhere near the comparable resources or spending available to their governments, is allowing citizens in their countries to live almost as long as those in high-income regions?
As we’ll see in the next few blogs - it’s largely about commitments to social policies which support public health, strong investment in health, particularly primary care, and ensuring the benefits of these programmes are felt equitably across their populations. In the next few articles then we’ll learn about how Cuba’s Polyclinicos Comunitarios and Medicina General Integral policies have applied social, preventative and integrated healthcare at a neighbourhood level, Brazil’s Family Health Strategy with its strong focus on community outreach, the Brigadista network in Nicaragua and Costa Rica’s Equipos Basicos de Atencion Integral de Salud (OK, so the last one is cheating a bit, as Costa Rica is a fairly wealthy country by Latin American standards, but you’ll see later why it’s included).
Throughout the blogs I want to make clear how much we could learn from health systems abroad if we gave ourselves the chance, the time, and the humility, to do so. So tune in tomorrow to learn more about some of these settings, and how we could integrate their approaches back home in the UK.
Jonny, Co-Director HCB Associates